Authors: Tamir Zitelny, MS4; Blake Briggs, MD; Mary Claire O’Brien, MD
Introduction
Status epilepticus is defined as one seizure episode lasting >30 minutes or multiple seizure episodes without a return to neurologic baseline/consciousness.1 Given the risks associated with this medical emergency, intervention should not be delayed. In this guide, we will focus on the approach to convulsive status epilepticus (CSE) in adults, a common form of status epilepticus, and the neurological sequela we look to avoid with prompt treatment.
Causes of status epilepticus
In patients without any prior diagnosis of epilepsy, the most common causes of CSE include an acute or subacute underlying cerebral pathology (such as a structural lesion, intracranial infection, stroke, or head trauma), a toxic/metabolic insult, or a combination of the two.2 In roughly 10% of these patients, status epilepticus may be the presenting manifestation of an underlying seizure disorder.3 In patients with a history of epilepsy, one of the most common causes is antiseizure medical nonadherence or subtherapeutic dosing of these medications.4-6
Presentation
Status epilepticus is a true medical emergency – its approach and consequences are remarkably different from “normal” or breakthrough seizures. Your approach must be significantly more aggressive.
Patients with CSE will demonstrate generalized, bilateral tonic-clonic movements in the setting of impaired mentation for greater than 5 minutes or will not return to baseline between repeated seizure episodes. This contrasts with other forms of status epilepticus which may exhibit more focal findings.7 The diagnosis of status epilepticus is clinical. CSE has the highest propensity for critical complications.7 Patients may demonstrate temporary neurologic deficits during the postictal period between or after seizure episodes (known as Todd’s paralysis).
When the patient is not seizing, do a solid neurologic exam. Specifically, note the patient’s alertness and orientation and examine for focal neurologic deficits. While EEG can often be diagnostic for CSE, in the ED setting, EEG should never delay intervention.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Once the patient is no longer seizing, a non-contrast head CT to assess for intracranial pathology is warranted, especially in those who have a first-time seizure. Consider a lumbar puncture in patients who have a fever and/or risk factors and whose presentation concerning for meningitis or encephalitis.8 Key lab tests include blood glucose levels, serum electrolytes, BUN, creatinine, WBC, Hgb, and toxicology studies. In patients with a known seizure disorder, serum levels of prescribed antiseizure medications are also useful in certain cases to assess for subtherapeutic intake.9-11
Early intubation?
If appropriate, rapid sequence intubation should never be withheld in an unresponsive, obtunded patient. To be clear, most patients who have an isolated seizure or even status epilepticus do not require intubation. They can often be ventilated and oxygenated during their seizure with a bag-valve-mask as needed. Most post-ictal patients quickly recover their respiratory drive. However, if there are signs of apnea and the patient cannot be appropriately ventilated and oxygenated during or immediately after their seizure, intubation is necessary.
Management
Like clockwork, we begin with addressing the “ABCs”: airway, breathing, and circulation. Some important interventions to keep in mind include:
- Maintain normoxia (i.e., O2 saturation > 95%)
- Begin transfusions as needed to maintain appropriate electrolyte concentrations
- Administer acetaminophen or cool febrile patients; consider external rewarming in hypothermic patients
- Correct hypoglycemia as needed
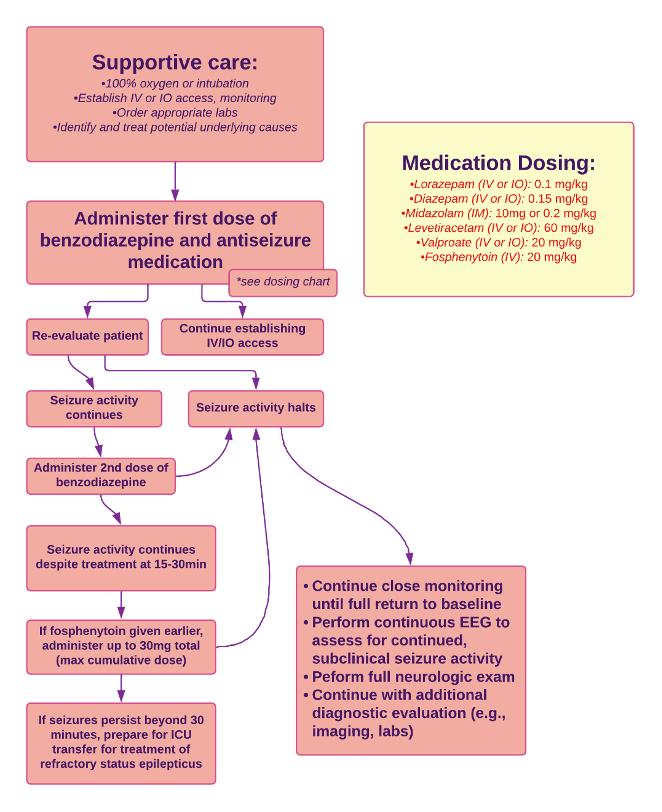
The primary goal of management is to halt seizure activity as quickly and safely as possible. This follows an algorithmic approach, giving supportive care and medications in a stepwise manner, as seen below.
First line medication is a benzodiazepine: diazepam, lorazepam, or midazolam (depending on available IV access).12-13
If unsuccessful after two doses, give an antiseizure medication: valproic acid, levetiracetam, or phenytoin/fosphenytoin.
The choice of medication is often based on whether the patient has a history of seizures and their current antiseizure medication profile. If a patient with a seizure history is found to be subtherapeutic, a loading dose of their current prescribed medication is appropriate.13 However, a serum antiepileptic medication level is wishful thinking in the ED.14-15 Thankfully, it’s been found that the three aforementioned medications are equally efficacious, with similar side effect profiles and rates of adverse effects.16 As such, any one of these medications is an appropriate choice.
After apparent seizure cessation, EEG (or repeat EEG if one was performed during the diagnostic process) is often useful to evaluate for CSE conversion to continued nonconvulsive seizures, particularly in patients whose mental status does not improve despite cessation of apparent seizure activity.17
Rapid seizure abortion in these patients is crucial. There is an indirect relationship between length of seizure activity and response to antiseizure medications. With delayed intervention, there is a risk for refractory status epilepticus (RSE), defined not by duration of seizure but rather as seizure activity that does not cease despite administration of two different antiseizure medications.18 In such cases – occurring in roughly 20% of patients with status epilepticus – immediate continuous EEG monitoring is indicated. If not already done, intubation is needed, along with emergency neurology consultation and transfer to ICU-level care for closer monitoring.18-22 Sedative infusions – such as propofol, pentobarbital, and midazolam – is the mainstay of treatment for RSE, making the ICU the most appropriate setting for seizure activity monitoring and maintenance of adequate ventilation and hemodynamics.
COMPLICATIONS
For patients experiencing their first episode of CSE, the mortality rate is roughly 16-20%, with the most important prognostic factors being age and underlying patient comorbidities.23-27 Other complications include cardiac arrythmias and cardiac injury (largely due to massive catecholamine release).28-30
Longer seizure duration is associated with worsening neurologic effects and decreased likelihood of reversibility. After approximately 30 minutes of seizure-like activity, neurologic effects notably worsen, with 10-50% of CSE patients left with long-term neurologic complications31. Further, in patients without history of a seizure disorder, roughly 40% will later develop epilepsy – a four times increased risk as compared to patients experiencing an acute, isolated symptomatic seizure.32-33
REFERENCES
- Guidelines for epidemiologic studies on epilepsy. Commission on Epidemiology and Prognosis, International League Against Epilepsy. (1993). Epilepsia, 34(4), 592–596.
- Barry, E., & Hauser, W. A. (1993). Status epilepticus: the interaction of epilepsy and acute brain disease. Neurology, 43(8), 1473–1478.
- Hesdorffer, D. C., Logroscino, G., Cascino, G., Annegers, J. F., & Hauser, W. A. (1998). Incidence of status epilepticus in Rochester, Minnesota, 1965-1984. Neurology, 50(3), 735–741.
- DeLorenzo, R. J., Hauser, W. A., Towne, A. R., Boggs, J. G., Pellock, J. M., Penberthy, L., Garnett, L., Fortner, C. A., & Ko, D. (1996). A prospective, population-based epidemiologic study of status epilepticus in Richmond, Virginia. Neurology, 46(4), 1029–1035.
- Coeytaux, A., Jallon, P., Galobardes, B., & Morabia, A. (2000). Incidence of status epilepticus in French-speaking Switzerland: (EPISTAR). Neurology, 55(5), 693–697.
- Fisher, R. S., Cross, J. H., French, J. A., Higurashi, N., Hirsch, E., Jansen, F. E., Lagae, L., Moshé, S. L., Peltola, J., Roulet Perez, E., Scheffer, I. E., & Zuberi, S. M. (2017). Operational classification of seizure types by the International League Against Epilepsy: Position Paper of the ILAE Commission for Classification and Terminology. Epilepsia, 58(4), 522–530.
- Trinka, E., Cock, H., Hesdorffer, D., Rossetti, A. O., Scheffer, I. E., Shinnar, S., Shorvon, S., & Lowenstein, D. H. (2015). A definition and classification of status epilepticus–Report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia, 56(10), 1515–1523.
- Dittrich, T. D., Baumann, S. M., Semmlack, S., De Marchis, G. M., Hunziker, S., Rüegg, S., Marsch, S., Tschudin-Sutter, S., & Sutter, R. (2021). Diagnostic yield of cerebrospinal fluid analysis in status epilepticus: an 8-year cohort study. Journal of neurology, 268(9), 3325–3336.
- Huertas González, N., Barros González, A., Hernando Requejo, V., & Díaz Díaz, J. (2019). Focal status epilepticus: a review of pharmacological treatment. Estatus epiléptico focal: revisión del tratamiento farmacológico. Neurologia, S0213-4853(19)30044-1. Advance online publication.
- Sánchez Fernández, I., Gaínza-Lein, M., Lamb, N., & Loddenkemper, T. (2019). Meta-analysis and cost-effectiveness of second-line antiepileptic drugs for status epilepticus. Neurology, 92(20), e2339–e2348.
- Müllges W. (2019). Diagnose und Behandlung des Status epilepticus auf der Intensivstation [Diagnosis and treatment of status epilepticus in the intensive care unit]. Medizinische Klinik, Intensivmedizin und Notfallmedizin, 114(5), 475–484.
- Brophy, G. M., Bell, R., Claassen, J., Alldredge, B., Bleck, T. P., Glauser, T., Laroche, S. M., Riviello, J. J., Jr, Shutter, L., Sperling, M. R., Treiman, D. M., Vespa, P. M., & Neurocritical Care Society Status Epilepticus Guideline Writing Committee (2012). Guidelines for the evaluation and management of status epilepticus. Neurocritical care, 17(1), 3–23.
- Treiman, D. M., Meyers, P. D., Walton, N. Y., Collins, J. F., Colling, C., Rowan, A. J., Handforth, A., Faught, E., Calabrese, V. P., Uthman, B. M., Ramsay, R. E., & Mamdani, M. B. (1998). A comparison of four treatments for generalized convulsive status epilepticus. Veterans Affairs Status Epilepticus Cooperative Study Group. The New England journal of medicine, 339(12), 792–798.
- Prasad, M., Krishnan, P. R., Sequeira, R., & Al-Roomi, K. (2014). Anticonvulsant therapy for status epilepticus. The Cochrane database of systematic reviews, 2014(9), CD003723.
- Silbergleit, R., Durkalski, V., Lowenstein, D., Conwit, R., Pancioli, A., Palesch, Y., Barsan, W., & NETT Investigators (2012). Intramuscular versus intravenous therapy for prehospital status epilepticus. The New England journal of medicine, 366(7), 591–600.
- Kapur, J., Elm, J., Chamberlain, J. M., Barsan, W., Cloyd, J., Lowenstein, D., Shinnar, S., Conwit, R., Meinzer, C., Cock, H., Fountain, N., Connor, J. T., Silbergleit, R., & NETT and PECARN Investigators (2019). Randomized Trial of Three Anticonvulsant Medications for Status Epilepticus. The New England journal of medicine, 381(22), 2103–2113. https://doi.org/10.1056/NEJMoa1905795
- Devinsky, O., Kelley, K., Porter, R. J., & Theodore, W. H. (1988). Clinical and electroencephalographic features of simple partial seizures. Neurology, 38(9), 1347–1352.
- Novy, J., Logroscino, G., & Rossetti, A. O. (2010). Refractory status epilepticus: a prospective observational study. Epilepsia, 51(2), 251–256.
- Brophy, G. M., Bell, R., Claassen, J., Alldredge, B., Bleck, T. P., Glauser, T., Laroche, S. M., Riviello, J. J., Jr, Shutter, L., Sperling, M. R., Treiman, D. M., Vespa, P. M., & Neurocritical Care Society Status Epilepticus Guideline Writing Committee (2012). Guidelines for the evaluation and management of status epilepticus. Neurocritical care, 17(1), 3–23.
- Mayer, S. A., Claassen, J., Lokin, J., Mendelsohn, F., Dennis, L. J., & Fitzsimmons, B. F. (2002). Refractory status epilepticus: frequency, risk factors, and impact on outcome. Archives of neurology, 59(2), 205–210.
- Holtkamp, M., Othman, J., Buchheim, K., & Meierkord, H. (2005). Predictors and prognosis of refractory status epilepticus treated in a neurological intensive care unit. Journal of neurology, neurosurgery, and psychiatry, 76(4), 534–539.
- Sutter, R., Marsch, S., Fuhr, P., & Rüegg, S. (2013). Mortality and recovery from refractory status epilepticus in the intensive care unit: a 7-year observational study. Epilepsia, 54(3), 502–511.
- Logroscino, G., Hesdorffer, D. C., Cascino, G., Annegers, J. F., & Hauser, W. A. (1997). Short-term mortality after a first episode of status epilepticus. Epilepsia, 38(12), 1344–1349.
- Neligan, A., Noyce, A. J., Gosavi, T. D., Shorvon, S. D., Köhler, S., & Walker, M. C. (2019). Change in Mortality of Generalized Convulsive Status Epilepticus in High-Income Countries Over Time: A Systematic Review and Meta-analysis. JAMA neurology, 76(8), 897–905.
- Aminoff, M. J., & Simon, R. P. (1980). Status epilepticus. Causes, clinical features and consequences in 98 patients. The American journal of medicine, 69(5), 657–666.
- Koubeissi, M., & Alshekhlee, A. (2007). In-hospital mortality of generalized convulsive status epilepticus: a large US sample. Neurology, 69(9), 886–893.
- Towne, A. R., Pellock, J. M., Ko, D., & DeLorenzo, R. J. (1994). Determinants of mortality in status epilepticus. Epilepsia, 35(1), 27–34.
- Manno, E. M., Pfeifer, E. A., Cascino, G. D., Noe, K. H., & Wijdicks, E. F. (2005). Cardiac pathology in status epilepticus. Annals of neurology, 58(6), 954–957.
- Simon, R. P., Aminoff, M. J., & Benowitz, N. L. (1984). Changes in plasma catecholamines after tonic-clonic seizures. Neurology, 34(2), 255–257.
- Hocker, S., Prasad, A., & Rabinstein, A. A. (2013). Cardiac injury in refractory status epilepticus. Epilepsia, 54(3), 518–522.
- Lothman E. (1990). The biochemical basis and pathophysiology of status epilepticus. Neurology, 40(5 Suppl 2), 13–23.
- Hesdorffer, D. C., Logroscino, G., Cascino, G. D., & Hauser, W. A. (2007). Recurrence of afebrile status epilepticus in a population-based study in Rochester, Minnesota. Neurology, 69(1), 73–78.
- Dodrill, C. B., & Wilensky, A. J. (1990). Intellectual impairment as an outcome of status epilepticus. Neurology, 40(5 Suppl 2), 23–27.



